Almost a million hip and knee replacements are at risk of cancellation, with an interactive map and health service briefings revealing where waits will grow and what national action is planned
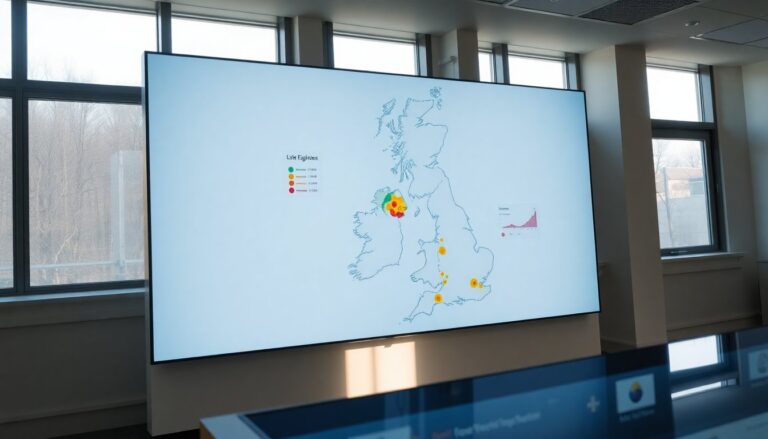
England’s NHS is bracing for a wave of cancelled and postponed hip and knee replacements after a major supply problem in orthopaedic materials collided with already-high demand for elective surgery. Estimates suggest as many as nearly one million procedures could be affected, and an interactive map published with regional data highlights where waiting lists are likely to swell.
NHS England has warned the situation needs urgent national coordination to limit harm to patients.
What the map and reports show
– The map and accompanying analysis reveal hot spots rather than a uniform national problem: places with heavy elective activity and local supply shortfalls face the steepest increases in cancellations.
Both cities and rural communities are on the list.
– Trusts received regional breakdowns identifying hospitals that may need to pause or reduce orthopaedic operating lists. Officials say a coordinated response is essential to avoid avoidable patient harm.
– Behind every statistic is a person whose life is limited by pain and reduced mobility.
Tens of thousands have already waited more than a year for joint surgery; further delays risk worsening physical and mental health and make daily tasks harder.
Why this is happening
– Two pressures have converged: a disruption in the supply of implants and consumables, and constrained elective capacity. Late deliveries—or missing items—can force entire theatre lists to be cancelled.
– Workforce shortages amplify the impact. Operating theatres can only run when sufficient trained staff are available; where staffing gaps and supply problems meet, waiting lists balloon fastest.
– Procurement and logistics bottlenecks have been localised, too. Some regions report shortages of particular implants, meaning cases are cancelled, rerouted or put on hold while hospitals scramble for alternatives.
What leaders are doing
– NHS England and trusts are rolling out contingency measures: targeted redistribution of existing stock, rerouting patients to less affected centres, accelerated procurement and stricter central reporting of inventories.
– Regulators are monitoring outcomes and waiting-list trends. Any substitute materials must meet safety standards, and clinical teams are being asked to balance the need to catch up with patient safety.
– Operational guidance encourages extending elective lists where possible, using unused weekend slots and deploying regional networks to transfer suitable cases. Still, long-standing issues—diagnostic backlogs, limited theatre time and staffing vacancies—limit how fast large numbers can be rebooked.
The limits of short-term fixes
– NHS England plans a targeted “sprint” with roughly £120m to boost elective activity before the financial year-end. That funding will help, but senior clinicians warn it won’t resolve persistent supply faults or close gaps where local theatres and staff are already overstretched.
– Short-term injections buy breathing space but sustainable recovery will need longer-term fixes: stable supply chains, more theatre capacity and a larger, better-distributed workforce.
Wider system pressures and inequality
– The problem doesn’t stop at implants. Diagnostic delays, rising referrals and limited imaging or pathology capacity slow preoperative work-ups and reduce throughput in theatres.
– Regional variation matters. Areas with older facilities, concentrated workforce shortages or fewer alternative providers are seeing sharper bottlenecks. The interactive map and recent waiting-time snapshots illustrate stark postcode-level differences in access and outcomes.
Patient impact and priorities
– Delays increase pain, limit mobility, may lead to muscle wasting, and can complicate later surgery—sometimes reducing the odds of a full recovery. They also add to patients’ mental-health burdens and everyday hardship.
– Clinicians stress strict prioritisation: urgent and time-sensitive cases must come first. Clear communication with patients about likely timelines and interim management options will be crucial to reduce anxiety and avoid avoidable deterioration.
Next steps
– Immediate: stabilise supply where possible, redistribute stock, open extra elective sessions, and use regional networks to move patients when safe.
– Medium term: shore up procurement routes, build contingency stock, expand diagnostic and theatre capacity, and recruit and retain perioperative staff.
– Long term: redesign supply chains for resilience, align surge measures with strategic planning, and improve transparency about waiting times so resources reach the worst-hit areas.
The National coordination, rapid local action and honest communication with patients are the only ways to limit cancellations and stop backlogs from worsening into a longer-term crisis. Trusts, suppliers and regulators will need to work in step to restore routine orthopaedic care while keeping patient safety front and centre.




